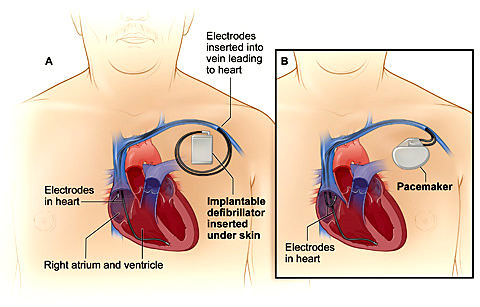
There are 3 treatment options for VT in patients with structural heart disease, although many patients require a combination: an ICD, antiarrhythmic medications, or catheter ablation. Many patients at risk for VT with structurally normal hearts are at risk of sudden cardiac death and as such are treated with an ICD. This is the most effective method of restoring a potentially life-threatening rhythm such as VT or VF back to a normal rhythm. However, an ICD does nothing to prevent the heart from going into VT. The ICD is a “safety net” and is like having an ambulance crew accompany you 24 hours a day. Please read our section on ICD.
Antiarrhythmic medications that modify the conduction of the electric impulse of the heart can be effective in suppressing VT. These medications can reduce the risk of recurrence by 75% but have potential side effects that include proarrhythmia, or worsening of the heart rhythm. For this reason, initiation of antiarrhythmic agents often requires close monitoring. Amiodarone, the most effective drug, has many side effects, which can involve toxicity to the vital organs like the liver, thyroid, lungs, eyes, and skin. Because of the discomfort associated with frequent ICD shocks and the side effects of antiarrhythmic drugs, catheter ablation is an important additional treatment option for many patients already using these therapies. The third treatment option is catheter ablation.
Radiofrequency catheter ablation was first described 20 years ago, it has played an increasing role in the treatment of ventricular arrhythmias. Initially used in the treatment of patients with multiple ICD shocks for VT (VT storm), it is now used more frequently and earlier in the management of VT, particularly in centers with a high volume of patients and experience. Catheter ablation is an excellent choice for patients when medications are not effective, tolerated, or preferred.
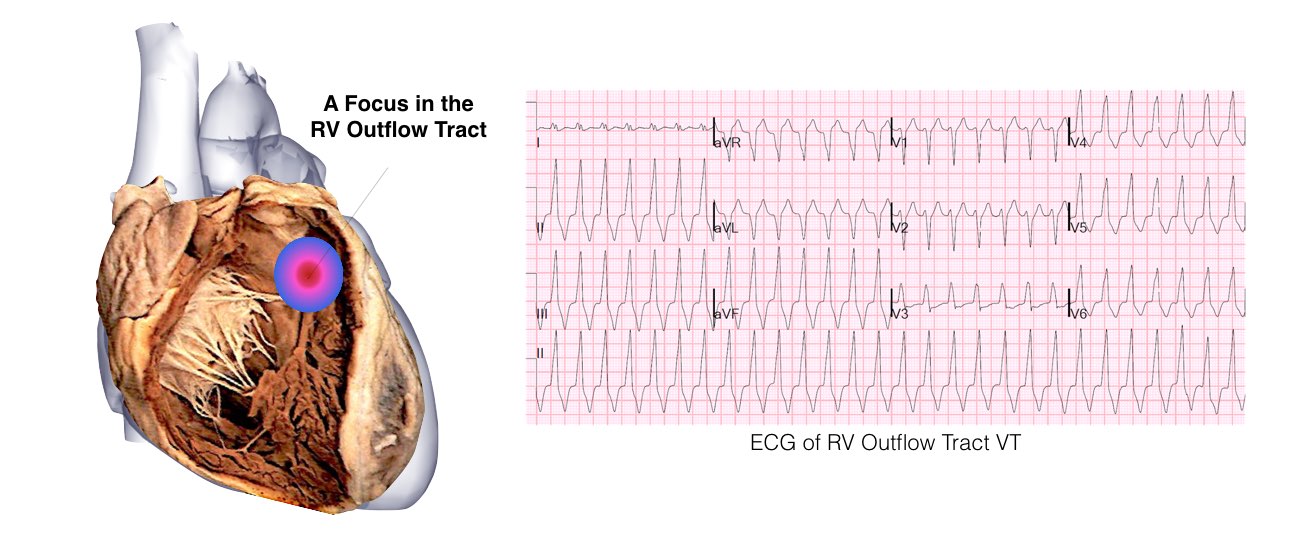
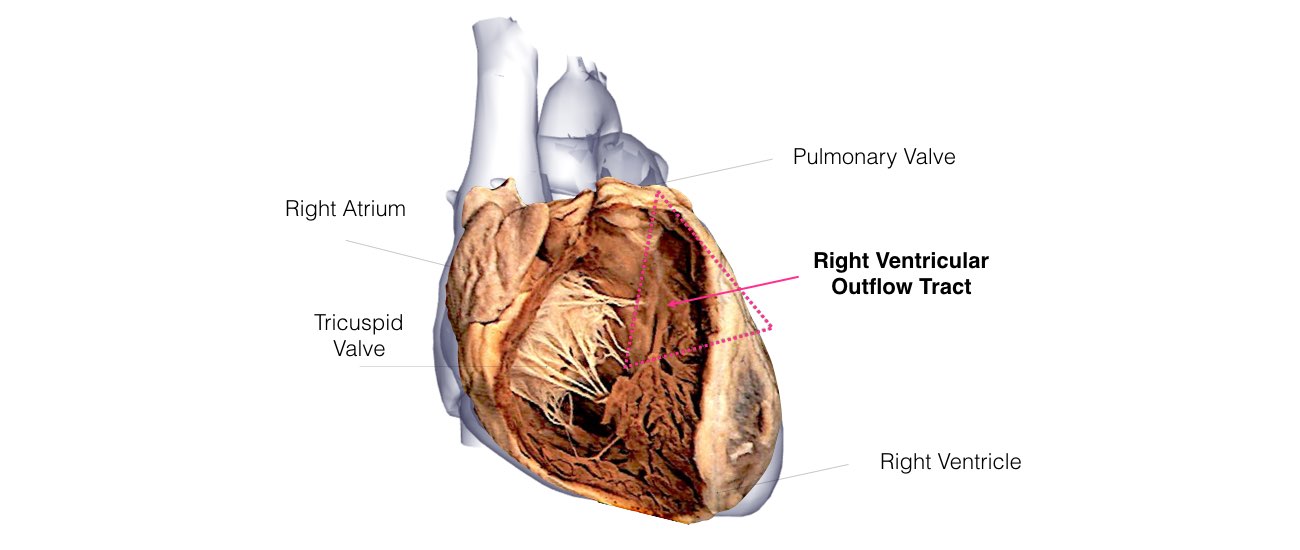
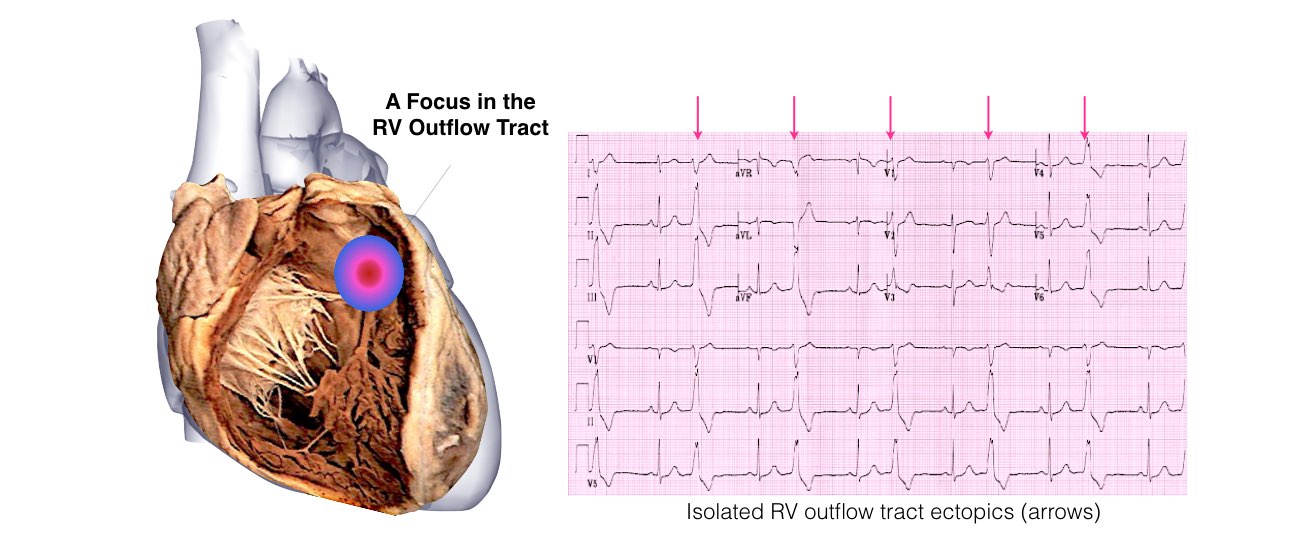
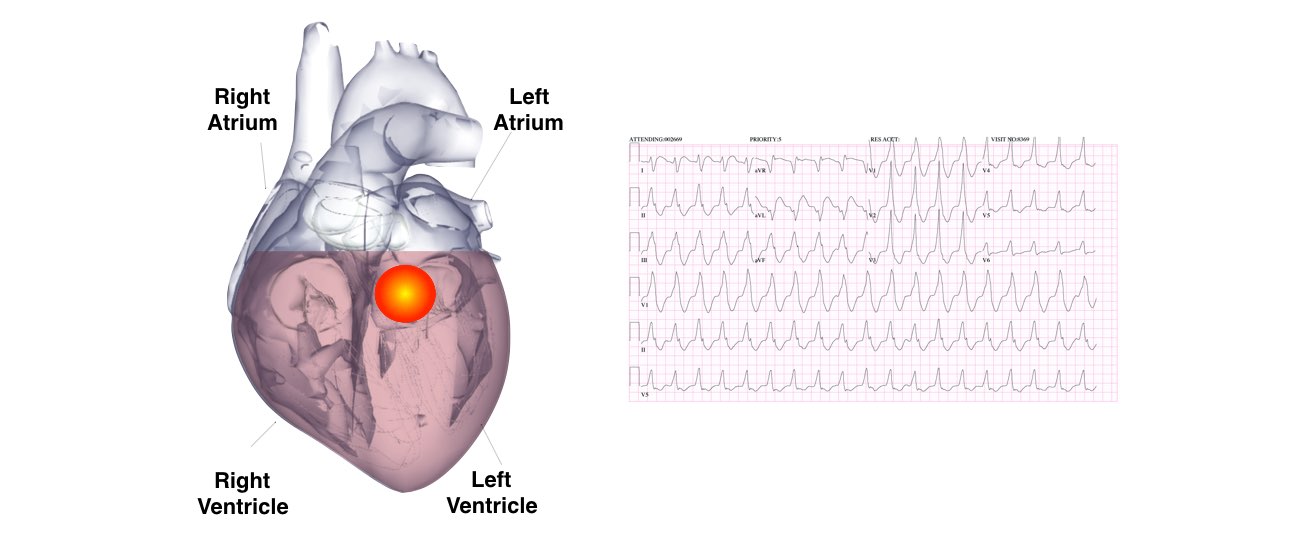
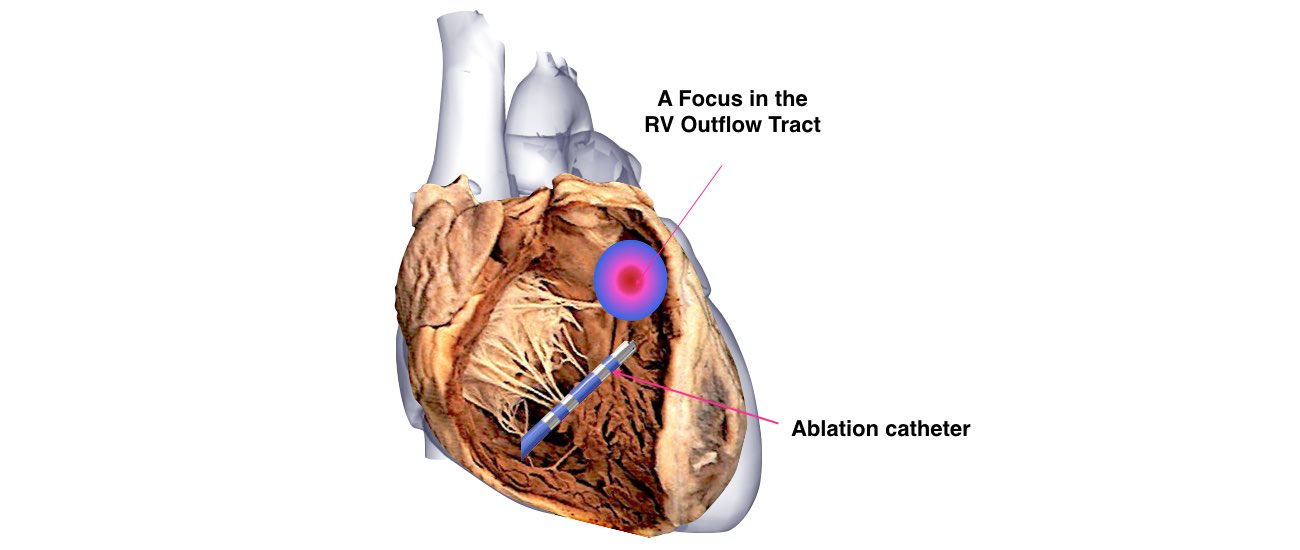
The aim of this procedure is to target the origin of the VT by placing a long, thin wire or catheter into the heart chambers through the veins of the leg. When areas that are critical to the VT circuit are identified, radiofrequency energy is applied to a small area (4 to 5 mm in diameter) to destroy the abnormal tissue. The number of burns required to treat the VT varies among patients. In patients with scar tissue in the heart, ablations may be performed within the scar and around its perimeter to cauterize or ablate the abnormal electric circuit responsible for the VT