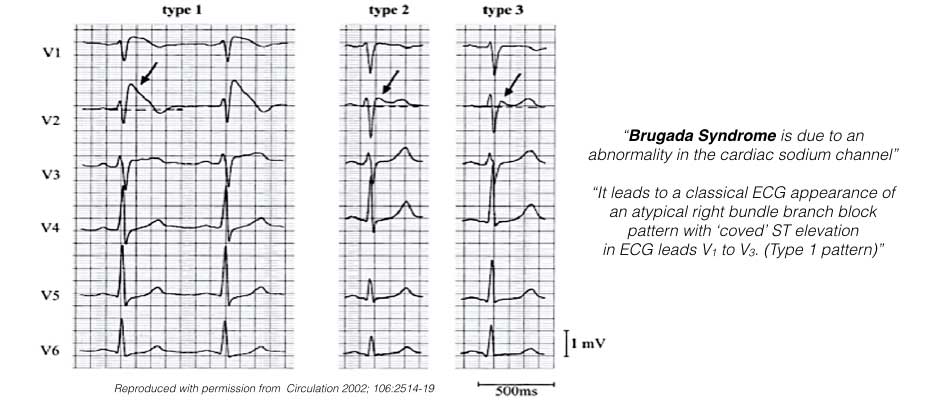
The diagnosis of Brugada Syndrome can only be considered when a diagnostic Type-1 Brugada pattern ECG occurs spontaneously or following drug provocation. The diagnosis is further confirmed when the ECG pattern occurs in conjunction with one of the following:
- Documented Ventricular Fibrillation (VF), polymorphic VT
- A family history of sudden cardiac death at <45 years
- A diagnostic Type-1 Brugada pattern ECG in family members
- Inducibility of VT during an electrical study
- Syncope or nocturnal agonal respiration (attributed to self-terminating polymorphic VT or VF).
Treatment of Brugada Syndrome depends on the risk of an abnormal heartbeat (arrhythmia) for that particular individual. Those considered at high risk have:
- A family history of sudden cardiac death
- A personal history of serious heart rhythm problems
- A personal history of severe fainting spells
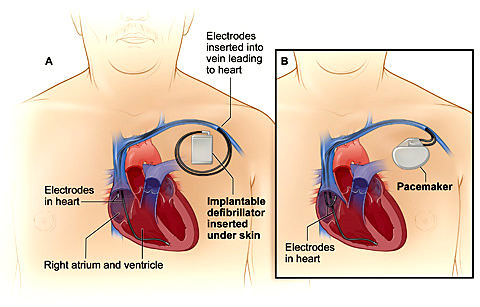
Implantable cardioverter-defibrillator (ICD). For high-risk individuals and symptomatic Brugada Syndrome patients, treatment may involve an Implantable Cardioverter-Defibrillator (ICD). An ICD is a small device continuously monitors your heart rhythm and delivers electrical shocks when needed to control abnormal heartbeats. The guidelines recommend ICD implantation in Brugada Syndrome patients who have survived cardiac arrest or have a history of syncope and documented ventricular arrhythmias.
There’s a small risk of complications from having an ICD implanted. People who have an ICD implanted as a treatment for Brugada syndrome have reported receiving shocks from their ICD even when their heartbeat was regular. These are called inappropriate shocks. This may be because many people who receive an ICD as a treatment for Brugada Syndrome are young, and may receive shocks when their heart rates increase during normal stresses, such as exercise.
Sometimes an inappropriate shock is delivered for another fast heart rhythm such as Atrial Fibrillation or an unrelated heart rhythm problem such as Supraventricular Tachycardia (SVT). Atrial Fibrillation occurs in about 20% of patients with Brugada Syndrome. Your doctor will program your ICD to reduce this risk. If you have an ICD implanted as part of your Brugada syndrome treatment, talk to your doctor about ways to avoid inappropriate shocks.
Drug Treatment
A drug called Quinidine is used in Brugada Syndrome patients who have repeated ICD shocks or an ‘arrhythmic storm’. Intravenous Isoprenaline (a form of adrenaline) is also helpful in the emergency treatment of arrhythmic storms in Brugada Syndrome.
As the changes of Brugada Syndrome on ECG are unmasked by febrile states, aggressive treatment of all febrile episodes is recommended with antipyretics like aspirin and paracetamol and cold sponges. Hypokalemia, large carbohydrate meals and alcohol and very hot baths have also been incriminated and should be avoided.
Drugs that can cause Brugada-like changes on the ECG are best avoided and include: Class 1antiarrhythmic drugs like flecainide, beta and alpha adrenergic blockers, channel blockers like verapamil, diltiazem, nifedipine, nitrates, potassium channel openers like nicorandil, tricyclic and tetracyclic antidepressants, phenothiazines and antidepressants like fluoxetine. Alcohol and cocaine can cause dangerous heart rhythms in patients with Brugada Syndrome. A website www.brugadadrugs.org gives a list of drugs to be avoided, preferably avoided and potential antiarrhythmic drugs in Brugada Syndrome.
Continued medical checkups. If you have Brugada syndrome, it’s a good idea to regularly check in with your doctor to make sure you’re properly managing your heart condition. Regular checkups can help your doctor decide if you need to change your treatment, and may help catch new problems early, if they occur.