You will receive a letter from the hospital bookings clerk or from the Doctors secretary outlining the date of your procedure and date and time of your admission to the hospital. In some cases a letter asking you to cease taking your medication is enclosed. This generally refers only to the medication you are taking for your abnormal heart rhythm. Your doctor will specify which medications he wants you to stop. These are usually stopped approximately 5 days prior to your procedure. If you are taking warfarin this will usually be continued but the dose may be varied in the days before the procedure based on your blood test results. If you are taking other blood thinners (Pradaxa, Xarelto or Eliquis) these would be stopped approximately 24-48 hours before the procedure and instructions will be provided.
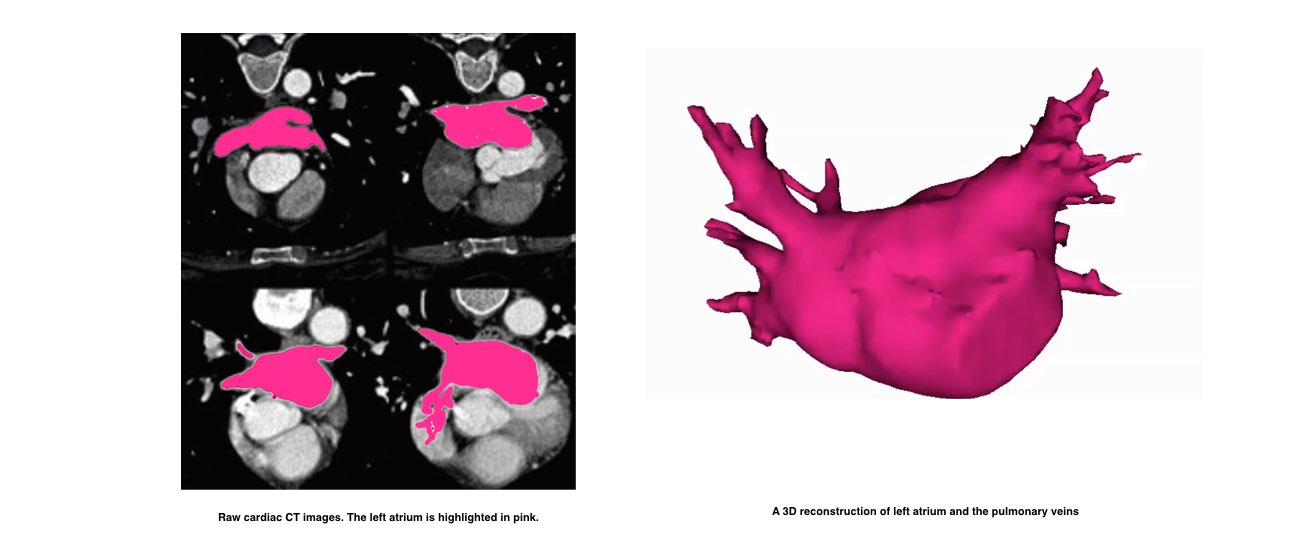
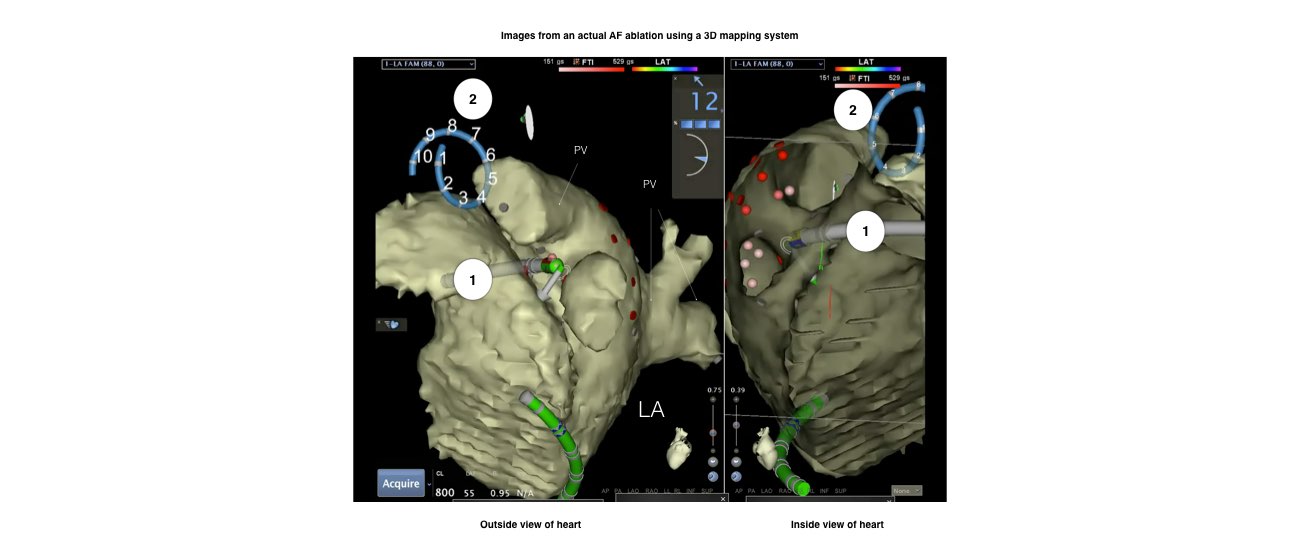
On the day before the procedure, a CT scan of your heart will be performed. This will be used during your ablation procedure.
Patients having the procedure at the Apollo Main Hospital, Chennai will be required to attend our Out-patient clinic on the day prior to your procedure where you will see a doctor who will record your medical history. You will also require an ECG and blood test. The doctor will also confirm the time you should be at the hospital for admission the following day.
You will be required to fast for at least six hours before the study. If your procedure is in the afternoon you may have a light early breakfast. If your procedure is in the morning, DO NOT EAT OR DRINK AFTER MIDNIGHT, except for a sip of water to help you swallow your pills.
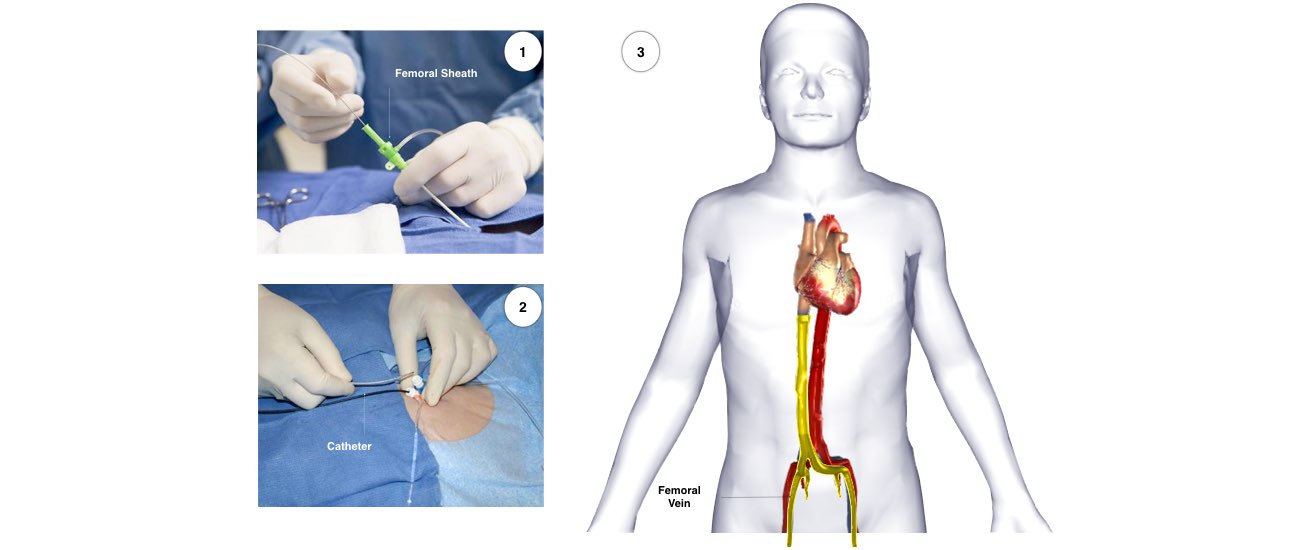
After the procedure you will wake up in a hospital ward called the recovery area. When you are completely awake you will be transferred to the normal hospital ward. You will have to lie flat for approximately 6 hours after the procedure. During this time, it is important to keep your legs straight and your head relaxed on the pillow. You will have a compression clamp on the groin area which stays in place for 4-6 hours. You will also have a urinary catheter which will be removed later that evening or the next morning.
It is usual to stay in hospital for 2 nights after the procedure. Your heart rhythm may be monitored during this time. During this time you will either continue warfarin or commence blood thinning injections. If you are taking Pradaxa, Xarelto or Eliquis, these will be restarted on the day you go home.
It is common to have a sore throat and some mild chest discomfort after the procedure. You will also have some discomfort and bruising in the groin (and neck area in the occasional case when the neck vein is required) after the procedure. This should usually improve over several days.
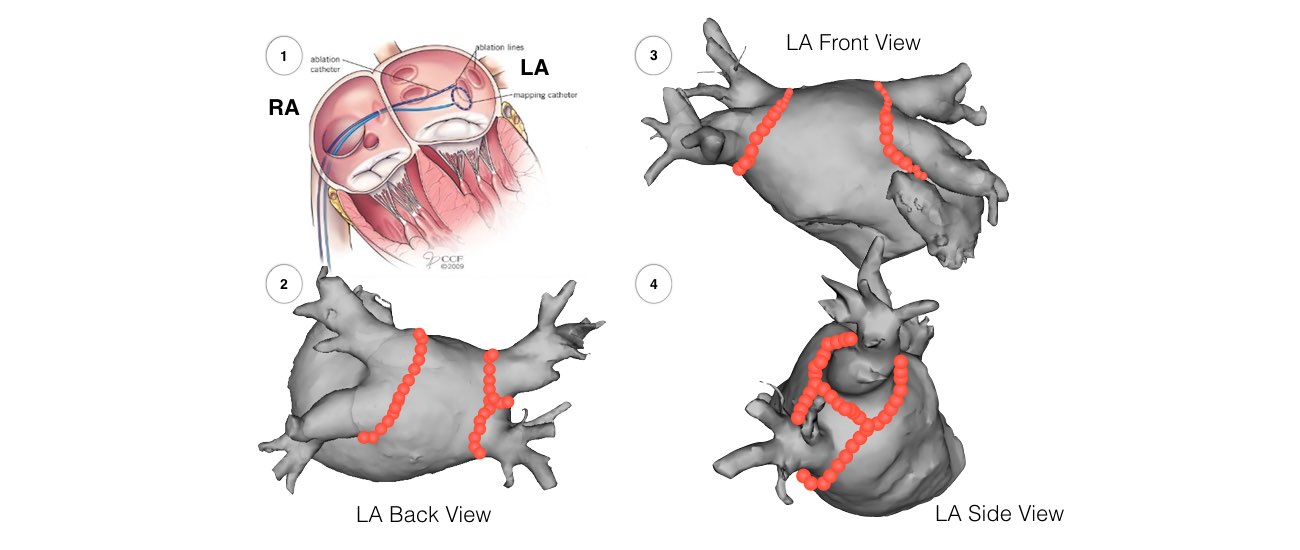
Because it takes several weeks for the areas of ablation to heal and form scars, it is not uncommon to experience abnormal or irregular heartbeat or rhythm for up to 4 weeks after the procedure. Rarely, atrial fibrillation may be worse for a few weeks after the procedure due to inflammation where the ablation was performed.
The majority of patients have approximately 1-2 weeks away from work.
After you go home, you will have an appointment for review with the consultant cardiologist who performed the procedure in the following 4-8 weeks.