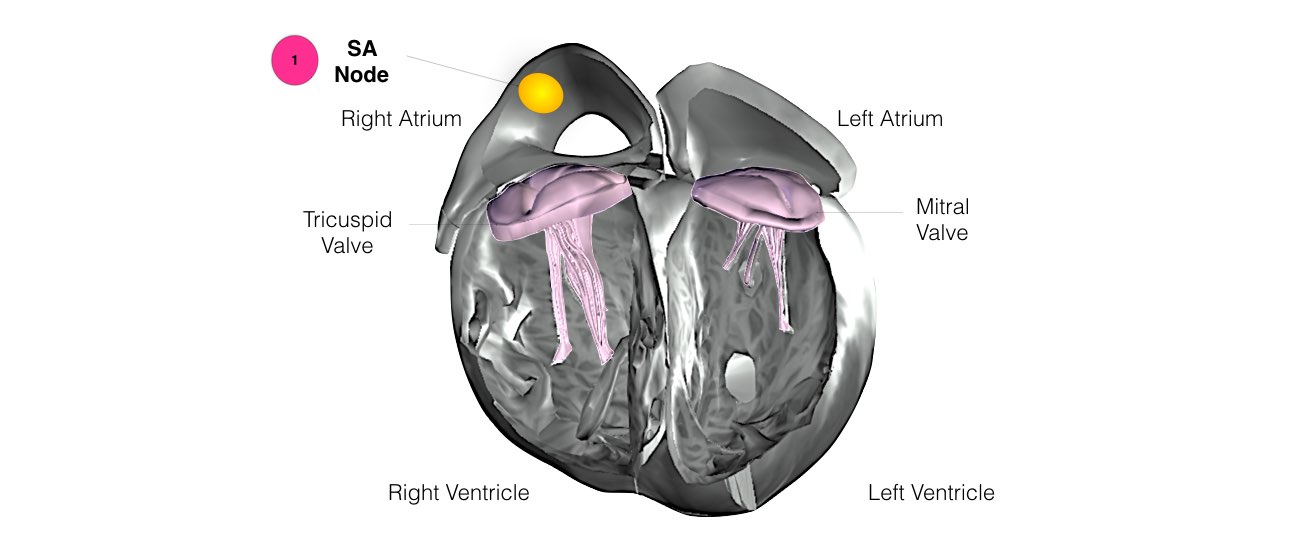
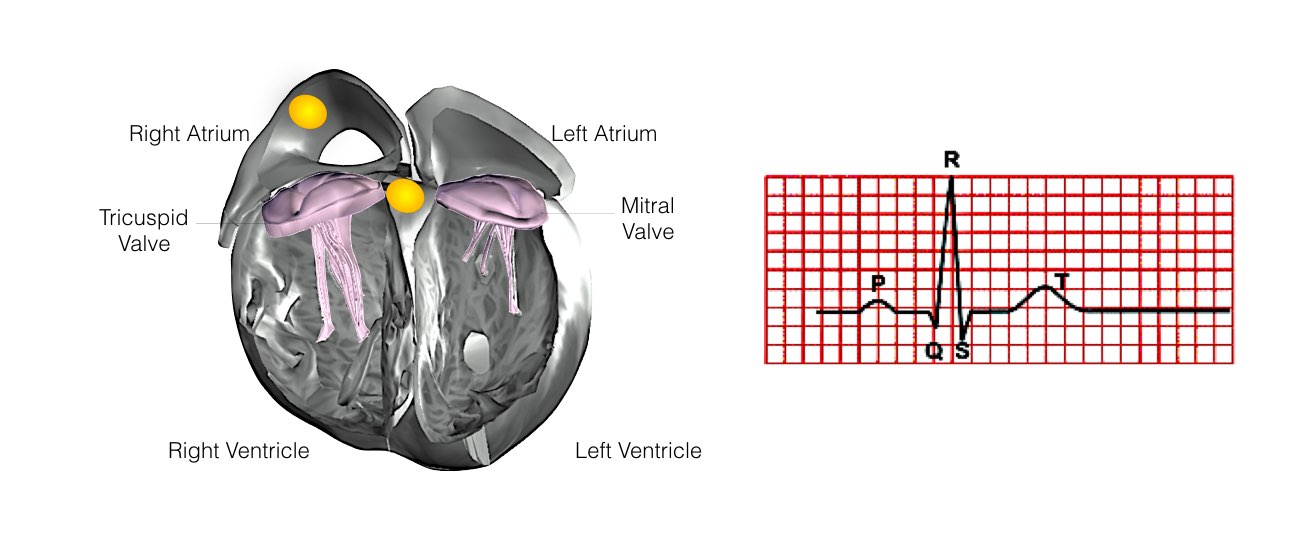
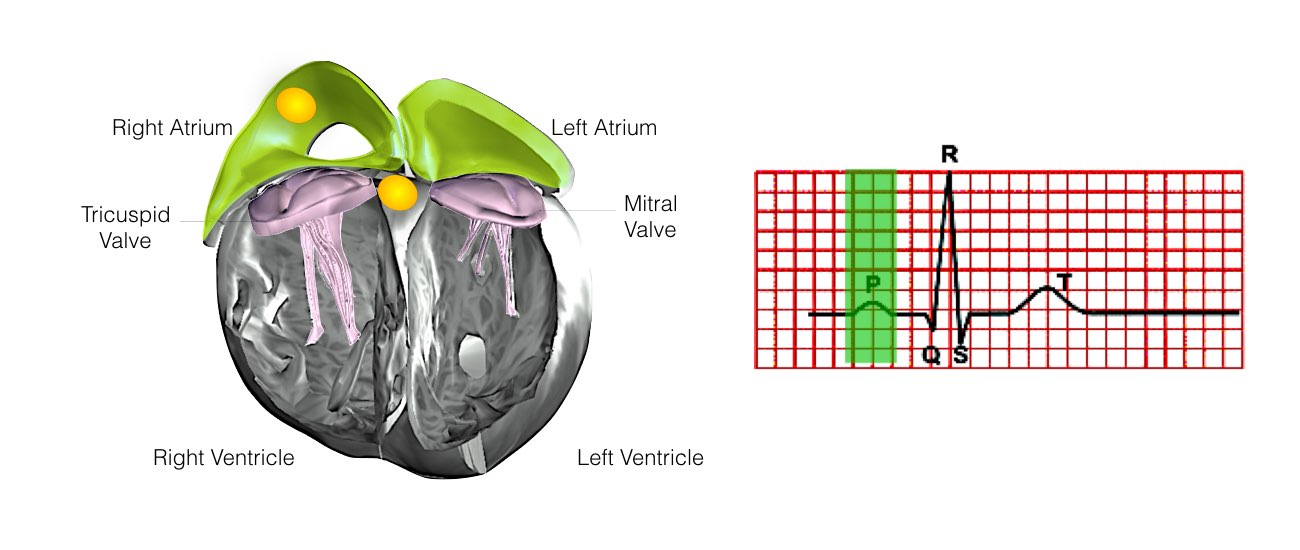
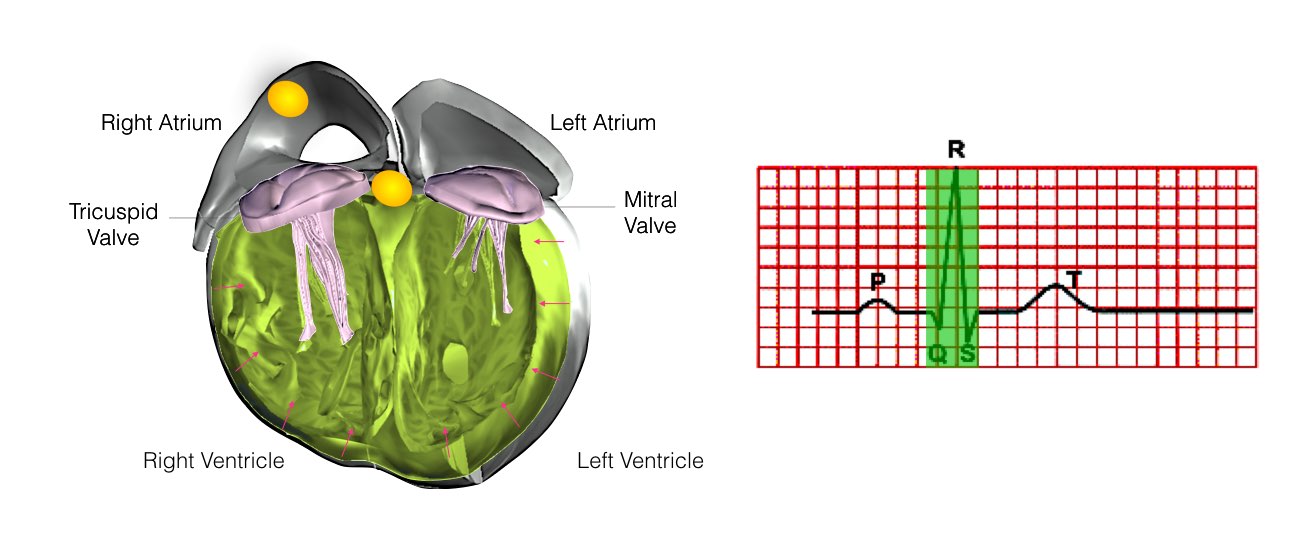
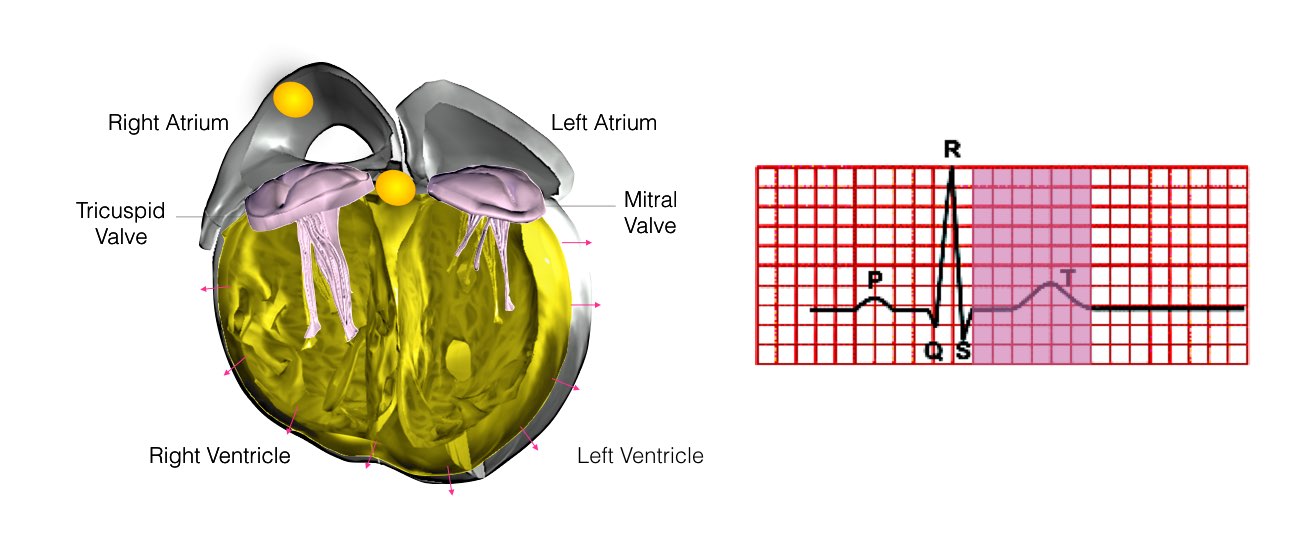
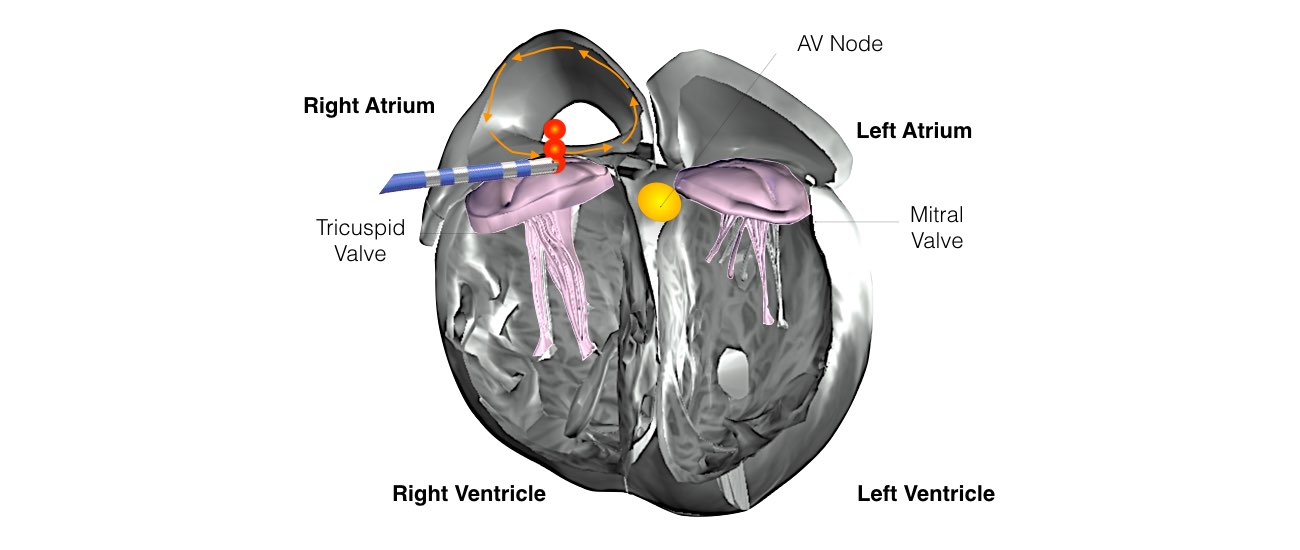
In order for the heart to do its work (pumping blood throughout the body), it needs a sort of spark plug or electrical impulse to generate a heartbeat. Normally this electrical impulse begins in the upper right chamber of the heart (in the right atrium) in a place called the sino-atrial (SA) node. The SA node is the natural pacemaker of the heart. The SA node gives off electrical impulses to generate a heartbeat in the range of 60 to 100 times per minute.
Menu
- Home
- About
- Learn
- Normal Heart Function
- Supraventricular Tachycardia (SVT)
- Ectopics / Missed Beats
- Bradycardia (Low Pulse Rate)
- Syncope
- Atrial Flutter
- Atrial Fibrillation
- Long QT Syndrome
- Brugada Syndrome
- Heart Failure
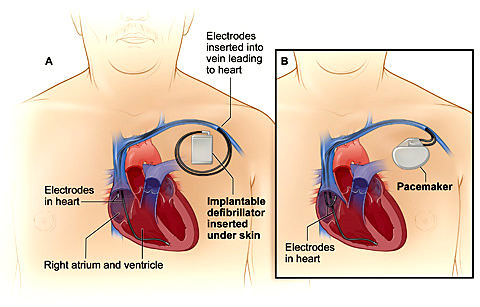
- Pacemaker
- Implantable Cardioverter Defibrillator (ICD)
- Ventricular Tachycardia in Normal Hearts (Idiopathic-VT)
- Coronary Artery Disease
- Ventricular Tachycardia in Structural Hearts Disease
- Services
- FAQs
- Media
- Contact
- Blog
close
Menu
- Diagnostic Tests
- Heart Rhythm Procedures
- Heart Rhythm Procedures
- Permanent pacemaker implantation
- Physiological Pacing
- Pediatric Pacemaker Implantation
- Leadless Pacemaker Implantation
- AV Node Ablation Plus Pacemaker Implantation
- Automatic Implantable Cardioverter Defibrillator (AICD) Implantation
- Cardiac Resynchronisation Therapy (CRT)
- Pacemaker and Defibrillator Extraction & Revision
- Implantable Loop Recorder (ILR)
- Coronary & Structural Cardiac Procedures
close