Insertion of a defibrillator is now a very common procedure. This is performed either under local anaesthetic with sedative medication to make you feel comfortable or under general anaesthetic. Your doctor will discuss this with you. The procedure takes approximately 1 hour and is performed in the cardiac catheter laboratory.
This is a special room that has a patient table, X-Ray tube, ECG monitors and other equipment. The staff in the lab will all be dressed in hospital theatre clothes and during the procedure will be wearing hats and masks.
Many ECG monitoring electrodes will be attached to your chest area. A nurse or doctor will insert an intravenous line usually into the back of your hand. This is needed as a reliable way to give you medications during the study without further injections. You will also have a blood-pressure cuff attached to your arm that will automatically inflate at various times throughout the procedure.
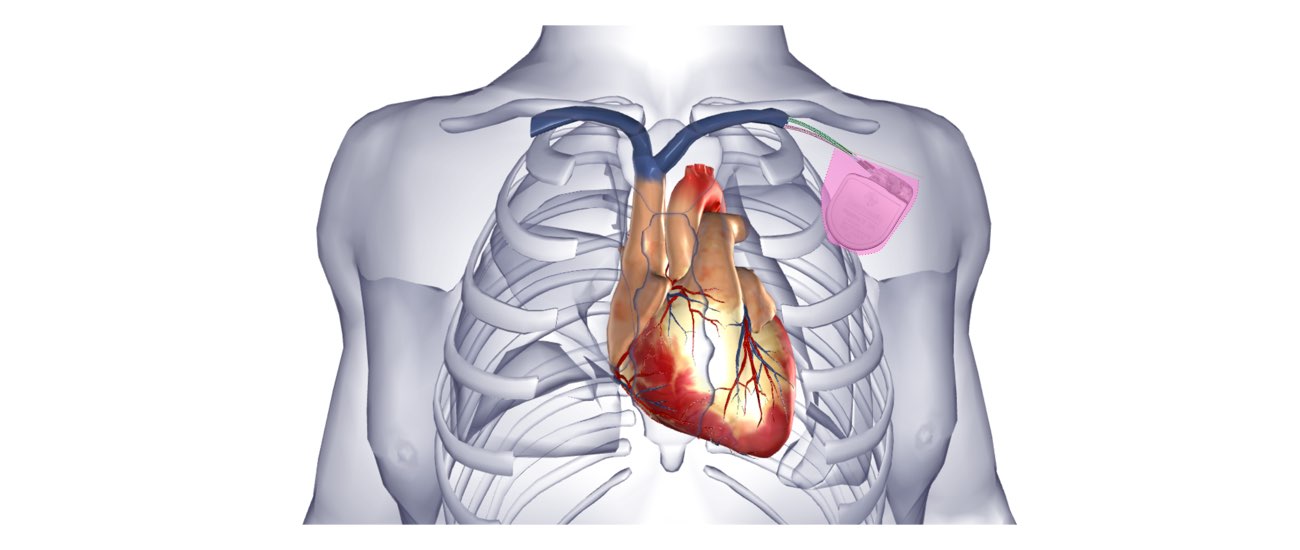
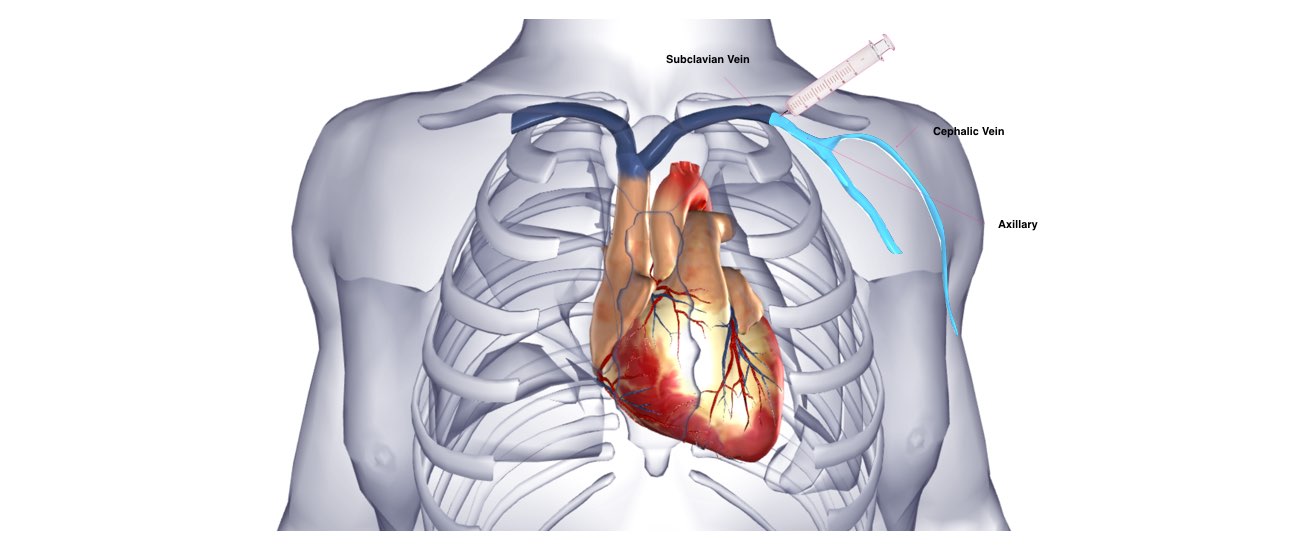
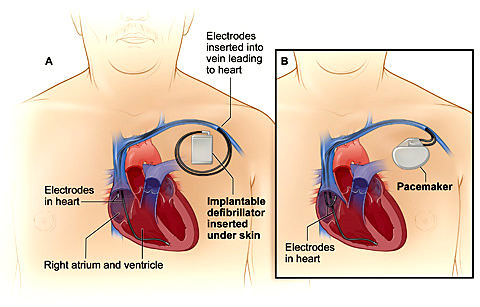
The defibrillator is inserted just under the collar-bone on the front of the chest, usually on the left side. The area is prepared with a special sterile solution that may feel cold. You will be covered by a large sterile sheet that will partly cover your face. You will be able to look out from under the sheet to the side and a nurse will be present at all times. You will be given oxygen to breathe by a small tube that is positioned under your nostrils or by a mask that covers your face.
At the start of the procedure, the doctor will inject local anaesthetic into the area under the collar-bone where the defibrillator is to be inserted. This will sting momentarily but the area will then be numb. During the procedure you may feel some firm pushing in the shoulder area but this should not be painful. If you experience pain or discomfort you should tell the nurse or doctor.
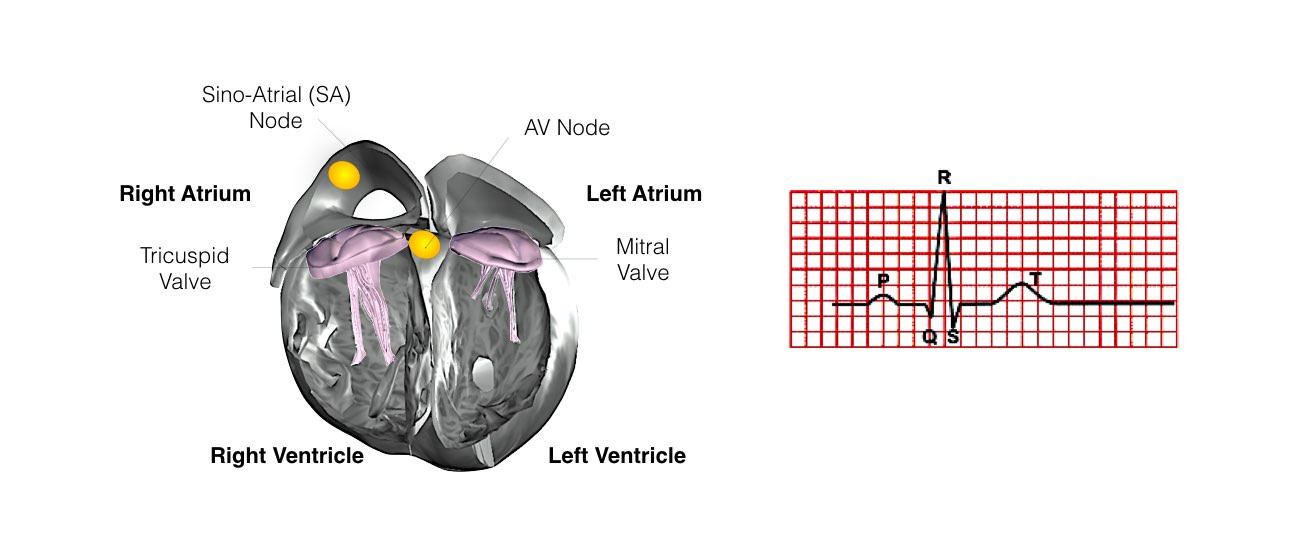
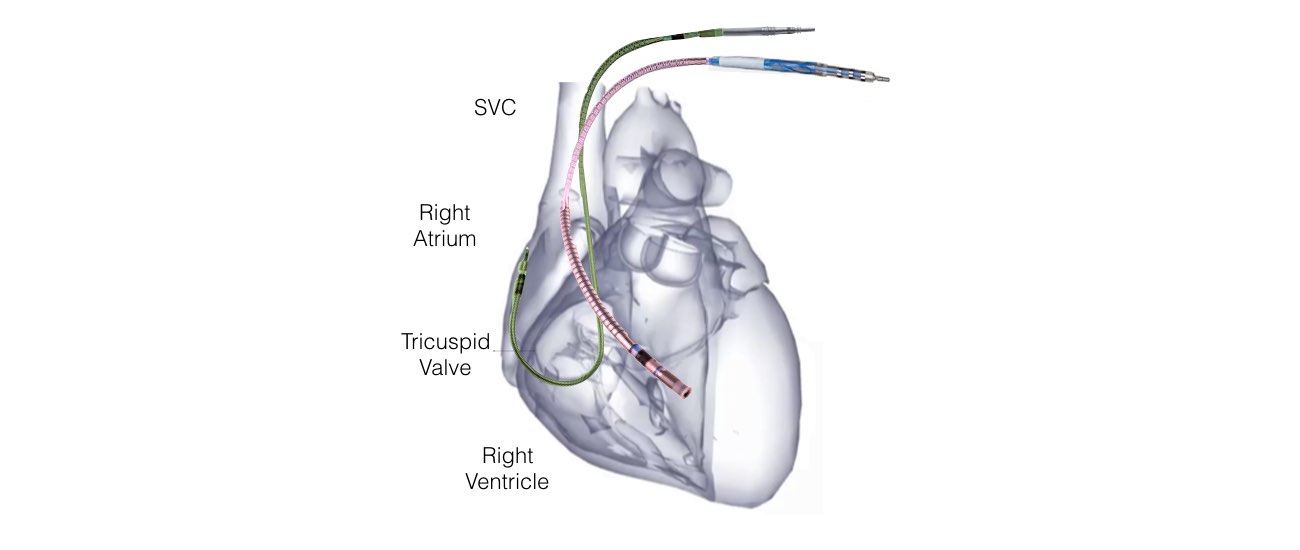
Usually 2 leads (special wires which connect the defibrillator with the heart) are inserted into the heart via the vein under the collarbone. These are manipulated into the heart under X-Ray control. Most commonly 2 leads are inserted, one into the right atrium and one into the right ventricle. These leads attach to the heart wall either with small hooks or with a small screw. Depending on your heart problem sometimes only 1 lead is inserted and on other occasions it will be necessary to add a third lead. Your doctor will discuss this with you.